Understanding Dry Eye Disease
Dry Eye Disease (DED) happens when your eyes don’t make enough tears, or when the tears don’t stay on the eye’s surface long enough.
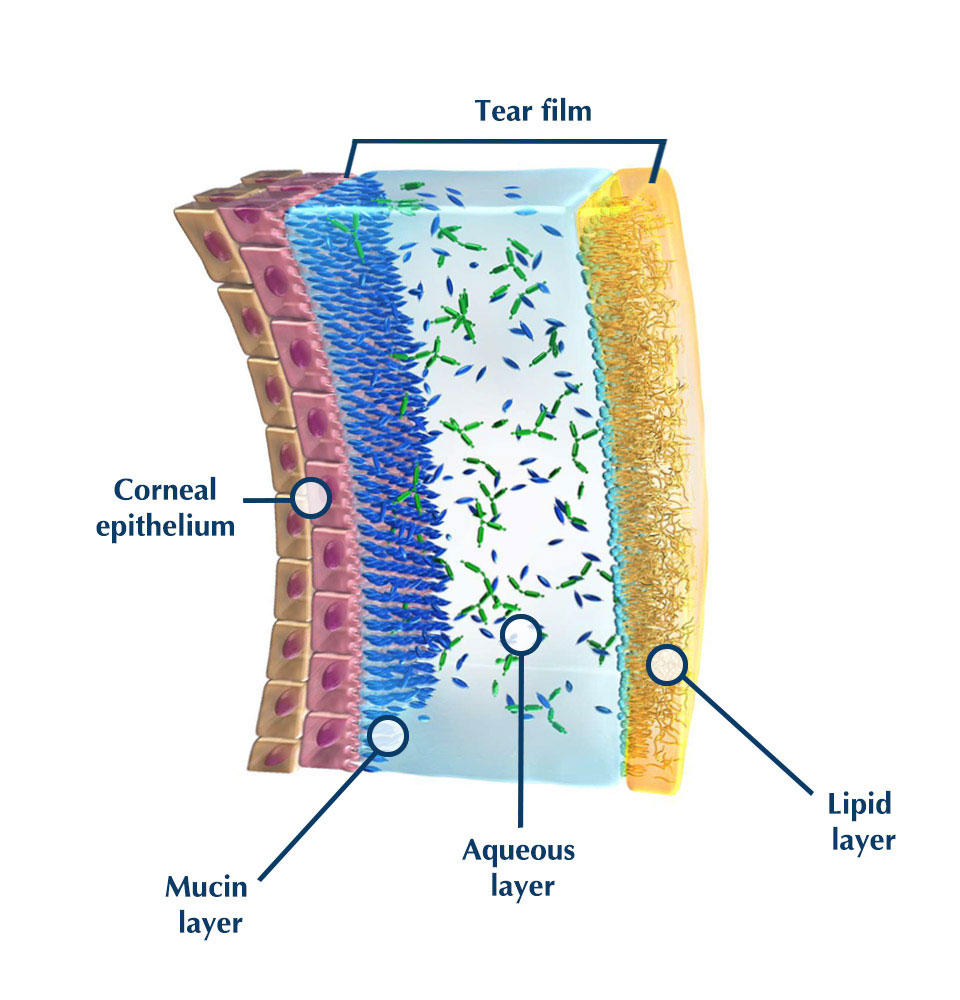
The tear film normally has three layers (oil, water, and mucin). If any layer is out of balance, your eyes can feel dry, gritty, or irritated.
Signs & Symptoms
- Stinging, burning, or scratchy eyes
- A sandy or gritty feeling
- Episodes of watery eyes (reflex tearing)
- Redness or soreness
- Blurred or fluctuating vision
- Heavy eyelids or eye fatigue
- Discomfort with contact lenses
- Difficulty reading or using a computer for long periods
Note: Sometimes watery eyes are actually a sign of dry eye — the eye floods with “reflex tears” that don’t lubricate properly.
Causes & Risks
Many factors can contribute to Dry Eye Disease, including:
- Age (more common over 40, especially in women after menopause)
- Medications such as antihistamines, blood pressure tablets, or antidepressants
- Autoimmune conditions (e.g., Sjögren’s syndrome, lupus, rheumatoid arthritis)
- Meibomian gland dysfunction (poor oil layer in tears)
- Prolonged screen use or infrequent blinking
- Contact lens wear or after laser eye surgery
- Environmental factors: air conditioning, wind, smoke

Treatment & Relief
Treatment depends on the severity and cause. Common options include:
- Artificial tears or lubricating eye drops (used regularly)
- Lid hygiene and warm compresses to improve oil gland function
- Prescription anti-inflammatory eye drops for more advanced cases
- Punctal plugs to reduce tear drainage
- Omega-3 supplements (fish or flaxseed oil)
- Lifestyle adjustments like blinking more, taking screen breaks, and wearing sunglasses outdoors
Quick Relief Tips:
- Blink often, especially at a computer
- Stay hydrated and use a humidifier if needed
- Remove all makeup before sleep
- Wear wraparound or UV-protective sunglasses outdoors
How Common Is It?
Dry Eye affects millions of people worldwide. It is especially common in women, people over 50, and those who spend long hours on digital devices. While often mild, severe cases can cause persistent discomfort and increase the risk of eye infections if left untreated.