Understanding Early Cataracts
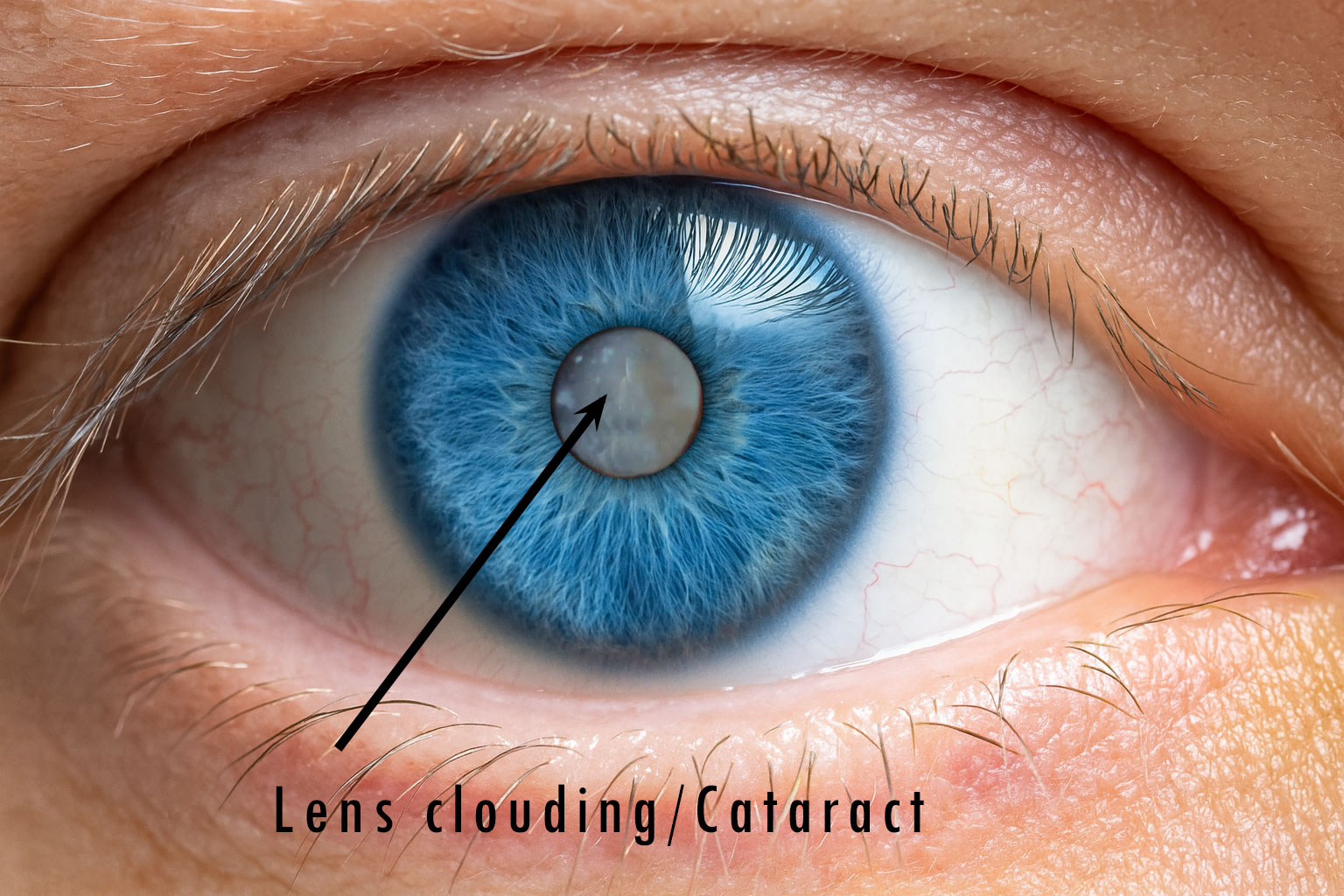
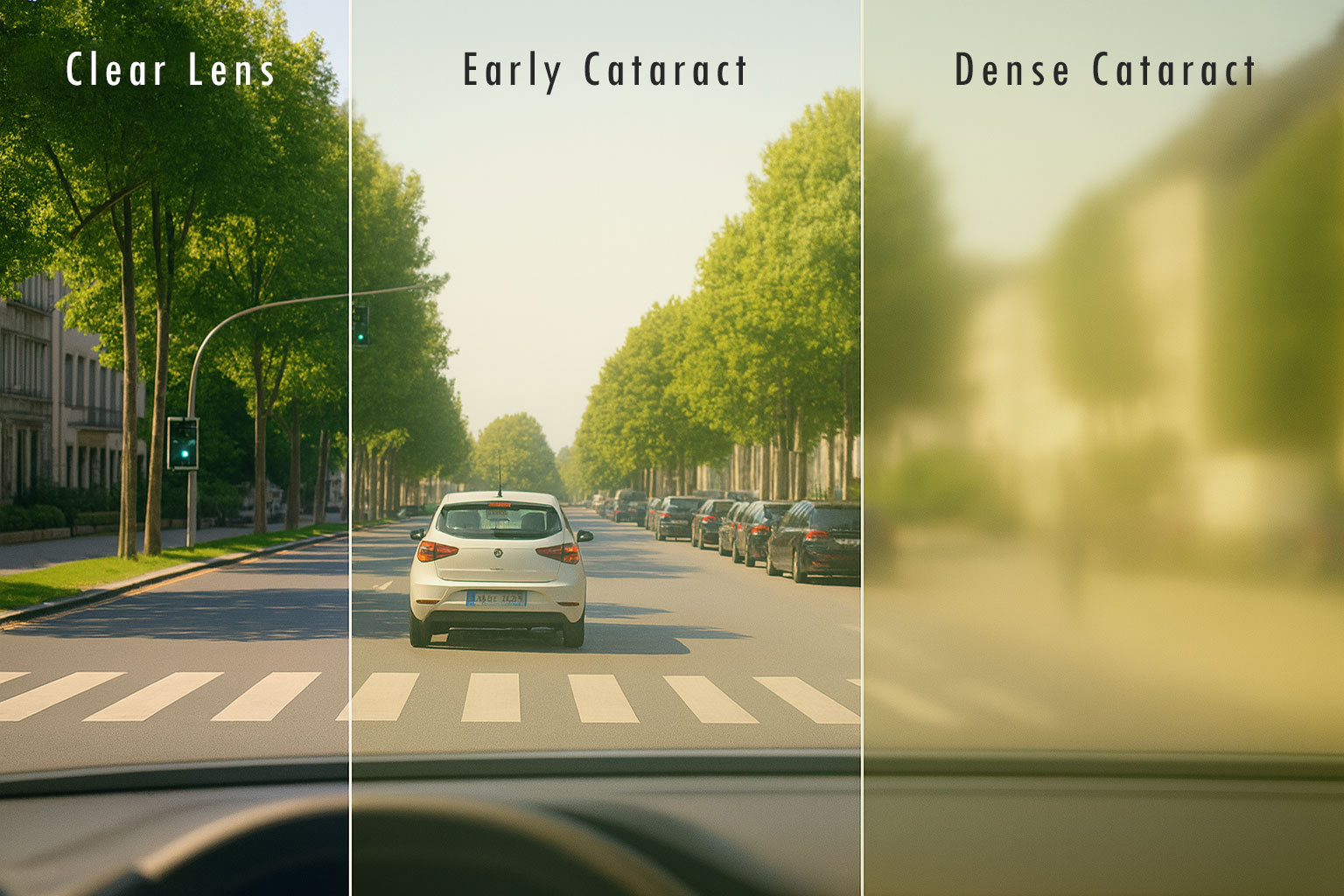
For your eye to see clearly, the lens must be transparent. With early cataracts, the lens becomes cloudy — often gradually — making your vision blurry or dull. You may notice trouble with contrast, colour, reading, or driving, especially at night.
Early Signs & Symptoms
- - Vision that’s blurry, cloudy, or filmy
- - Colours seem faded or less vibrant
- - Increased glare from sunlight or headlights
- - Halos around lights at night
- - Frequent spectacle prescription changes
- - Feeling like your glasses are always “dirty”
- - Trouble seeing well with glasses or contact lenses
Note: These symptoms can overlap with other eye conditions. If you're experiencing them, a professional eye exam is essential.
What Causes Cataracts?
Inside your eye, the natural lens is made mostly of water and proteins arranged in a way that keeps it crystal clear. As we age, some of these proteins begin to break down and clump together, forming cloudy patches known as cataracts. Over time, these patches can grow and scatter light, making vision blurry or dull.
Most cataracts progress gradually and can be monitored without the need for immediate surgery. However, understanding the type and cause helps your optometrist recommend the best approach for managing your vision.
Risk Factors
While the most common type — called age-related nuclear cataracts — develops slowly over many years, there are actually several different types. Some cataracts form after eye injuries, others appear in people with diabetes, and some can even be present from birth (congenital cataracts). Certain medications like corticosteroids may also accelerate cataract formation.
Other risk factors include:
- - Advancing age
- - UV radiation (sun exposure)
- - Diabetes, hypertension, obesity
- - Smoking or heavy alcohol use
- - Long-term use of steroids or statins
- - Eye injuries or previous surgery
- - Family history of cataracts
- - High myopia (severe short-sightedness)
Do Cataracts Always Need Surgery?
No. In many cases, people live comfortably for years with early cataracts. Better lighting, updated glasses, or anti-reflective coatings can help improve your vision in the meantime. Surgery is only recommended when cataracts begin to impact your daily life.
Helpful Advice
- - Have regular eye exams to monitor cataract progression
- - Improve lighting at home and work
- - Wear sunglasses with full UV protection
- - Use anti-glare lenses for night driving
When to Consider Surgery
Cataract removal is never an emergency. Surgery is typically discussed when vision loss affects work, hobbies, or safety (like driving at night). If you're unsure, your optometrist will guide you — but the final decision is always yours.
Note: Your optometrist may detect early cataracts many years before surgery is necessary. Regular visits ensure timely advice without rushing into surgery.
Tips for patients considering cataract surgery
Before your cataract or refractive lens exchange surgery, ask your optometrist to guide your ophthalmologist on the most suitable intraocular lens (IOL) selection.
As a vision specialist, your optometrist knows your day-to-day visual needs, lifestyle habits (reading, driving, digital work), and previous eyewear preferences. By sharing this insight with the ophthalmologist, it helps ensure that the IOL choice aligns with your real-world expectations.
This collaboration reduces the risk of post-surgery surprises, like still needing glasses more often than expected or not achieving the clarity you hoped for.
Global Impact
Cataracts account for over 50% of global blindness, especially in areas with limited access to surgery. In developed countries, long surgical waitlists can still delay treatment — making early detection and management important.
